The complex process of implantation - a biological and immunological paradox(1)
In my view the answer to the question raised by Raymond regarding the undetected actions of this drug regime is to be found both at a gene transcription level and within the domain of the delicate balance that typifies the maternal endometrial immune and communication systems.
Research by Piccinni (2007) highlights the complex interplay between various immune regulating chemicals at the fetomaternal micro-environment leading up to implantation, as the following quote attests.
"It is apparent that an immunological mechanism may play a role in pregnancy and embryo development." Amongst the vital factors (technically known as cytokines) listed by Piccinni are IL-4, IL-10, M-CSF and LIF which are produced "at the fetomaternal interface" and "could contribute to the maintenance of pregnancy." Interestingly this researcher reported that these crucial pro-implantation immune factors were produced both by the cellular envelope (known as the cumulus oophorus) which surrounds the oocyte "during ovulation" and also the embryo prior to implantation.
The oocyte activity clearly implies a purposeful intent to promote implantation should fertilization occur. The author also states: "Our results show that hormonal influences seem to play a critical role in determining the T-cell cytokine pattern at the fetomaternal interface and in the cumulus oophorus." (2)
A number of essential aspects of the work by Piccinni require expansion.
First, Piccinni specifically noted that progesterone is a potent inducer of the four pro-implantation cytokines previously mentioned (also know as Th2-type cytokines). These cytokines must be produced in sufficient quantities otherwise the human embryo will be rejected by another group of cytokines, called the Th1-type. The pro- and anti-implantation groups are engaged in a style of immune competition. Insufficient levels of the Th2-type cytokines - controlled by progesterone - results in immune rejection by the Th1-type of cytokines. Why? Because the embryo is comprised of genetically foreign DNA. This process of rejection is called allograft rejection.(3)
Second, the balance between these two competing groups of cytokines determines the sustainability of the pregnancy. Piccinni has shown that in women who experience unexplained recurrent abortion (URA) there are defective levels of LIF, M-CSF, IL-10 and IL-4 .
Third, it is reasonable to postulate that the supra-physiological levels of levonorgestrel (a progestin) used in the Yuzpe method could alter the finely tuned balance between pro- and anti-implantation cytokines. Indeed, Piccinni has stated that "our results show that hormonal influences seem to play a critical role ..." in determining the patterns of the essential cytokines. (4)
Joined to these anti-implantation actions are other delicate molecular aspects to the processes of implantation which have been considered as potential attack points for post-coital drug regimens. Precisely how these actions exert their influence is an emerging field of research and conflicting data exists.(5) Furthermore, as research technologies become more sophisticated, some earlier conclusions apropos of the mechanisms of action of post-coital drugs and devices are subject to modification, clarification or rejection.
Vital to this discussion is the overarching fact that these implantation factors are, in-vivo, regulated either directly or tangentially by ovarian-derived estrogen (E2) and progesterone (P4). Therefore, it is biologically plausible to expect that synthetic estrogens and progestins, such as those found in contemporary formulation of the daily birth control pill, and administered at higher doses as a 'morning-after' treatment, would also adversely influence various implantation factors. This is a reasonable expectation for two reasons.
First, the synthetic hormones present in the once-a-day birth control pill bind to and interact with the same receptors that natural estrogen and progesterone attach to. The receptors have the task of receiving the respective hormones, rather like a lock (the receptor) receives a key (the hormone), resulting in a biological effect. This hormone/receptor interaction is one of the foundations upon which the birth control pill was developed. Because of this mutual affinity for the same receptors, it is not surprising to find that the artificial female hormones can mimic, or even disrupt the normal cyclical patterns within the endometrial environment.
Second, when a woman takes the dosage regimen according to the Yuzpe method, she is ingesting a dose seven-fold greater than she would ingest when taking the once a day birth control pill. (6)
Given that research has revealed how the daily pill format negatively interferes with the complex array of events necessary for implantation of the human embryo, it is pharmaceutically logical to conclude that a sudden, seven-fold intake of the same hormones would likewise impact adversely on the delicate process of implantation. The earlier mentioned findings by Raymond et al (2000) support this conclusion. The following discussion will review newer research findings which highlight the possible attack points at which the Yuzpe method of pre-implantation/emergency 'contraception' could be operative.
Initially, these hormones could interfere with the mandatory bio-chemical communication between the embryo and the maternal endometrium prior to implantation. This precise, structured maternal/embryo communication has been varyingly referred to as "a signalling system",(7) embryonic "dialogue", (8) "molecular communication" (9) and "cross-talk." (10) Piccinni has summarised the complexities of the pre-implantation process as requiring "exquisite dialogue"(11) between the human embryo (at the blastocyst stage), and the maternal endometrium. Analogously, this process could be likened to the communication between a spacecraft and mothercraft prior to docking.
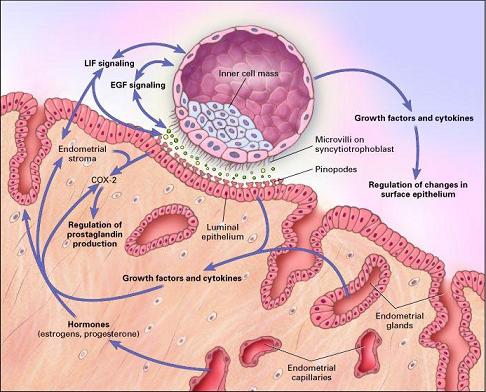
The human blastocyst at the feto-maternal microenvironment.
Signalling and implantation system. Reproduced with permission. (12)
The interleukin system is an indispensable component of pre-implantation embryo/endometrial communication. Inappropriate levels of female hormones or the ratio between the two has been shown to have a detrimental affect upon this implantation factor at the critical stage of alignment of the human embryo with the receptive cells of the endometrium prior to implantation, a "docking" style operation known as apposition.(13) As previously discussed, the Yuzpe method obviously meets the criteria of 'inappropriate levels'.
Sequentially associated with embryo/maternal cell-talk is the requirement for holding structures to be adequately present on the surface of the endometrium. These structures will maintain proper embryo/endometrial cellular contact whilst the embryo completes the implantation process. This life sustaining attachment/implantation process is, in part, dependant upon the adequate expression of cell adhesion molecules known as integrins. Integrins are maximally present on the surface of the endometrium on the 6th day after ovulation. This day marks the "opening of the implantation window." (14) Integrins could be considered to have the task of operating as docking clamps.
Regular use of the daily pill has been shown to down-regulate the activity of integrins, notably the αvβ3 class, thereby minimalising the possibility of successful implantation. (15) It is reasonable to hypothesize that substantially higher dose of the pill, as a post-coital pre-implantation/emergency regimen would be even more deleterious to the levels of integrin expression. Consequently, implantation would be imperilled.
Evidence is also emerging that other endometrial structures, such as pinopodes and osteopontin, also play a vital role in implantation. These attachment factors are present to an adequate level only during the "window of implantation" days.(16) (17) Pinopode levels are increased by natural progesterone, and decrease under the influence of natural estrogens.(18) Fully developed pinopodes are only present on the endometrium for a period that does not exceed 48 hours, their levels vary from patient to patient and they are "affected by hormonal treatment." (19)
This life cycle of less than 48 hours must be recalled when reading papers that claim that various forms of PCC do not affect pinopodes levels. The study may simply have been conducted outside of the narrow frame of pinopode presence.
Leukemia inhibitory factor (LIF) has also been confirmed as vital to embryo attachment and implantation. (20) An excessive plasma level of progesterone has been shown to decrease LIF levels 2.3 fold, thereby impeding implantation. An excessive level of estrogen has also been shown, in mice, to significantly stimulate LIF production. Paradoxically, too high a level of LIF is also disadvantageous to implantation, due to LIF-induced endometrial under-development.(21) Excessive levels of synthetic female hormones are a trademark of the Yuzpe method; hence interference with implantation, via damage to the proper levels of pinopodes, osteopontin and LIF is biologically plausible.
Insulin-like glucose factor-1 (IGF-1), insulin-like glucose factor-II and their related binding protein also have a confirmed, vital role in implantation, (22) and their influence on fetal development begins prior to implantation. (23) These implantation factors are under hormonal control (24) and daily use of the birth control pill has been shown to increase the levels of the binding protein (IGFBP-I) (25) (26) and decrease the levels of IGF-I.(27) Research indicates that excess levels of IGFBP are possibly implicated in shallow implantation and subsequent premature pregnancy loss. (28) The Yuzpe method of supra-physiological synthetic hormones ingestion would be expected to have an adverse impact on IGFBP similar to, if not greater than that seen with the daily pill. Clearly, as this research indicates, implantation is not akin to two pieces of sticky Velcro randomly touching and adhering to each other.
One final aspect of the Yuzpe method's mechanism of action requires consideration - does this method alter the time of ovulation, and if so, what relevance does this hold from a bio-ethical perspective? Research has shown that when taken before ovulation, Yuzpe can cause a delay in ovulation, of 1-10 days duration. A delay of one day would still permit fertilization. But implantation in these instances is unlikely because in these same women, a premature period was induced.(29)
More recent analysis has sought to quantify the degree to which the Yuzpe method truly acts as a contraceptive, that is, by its action upon ovulation. Research by Mikolajczyk and colleagues (2003) has reported that disturbances to ovulation perhaps account for "a little above 50%" of the mechanism of action of the Yuzpe method, and infer that other actions, including impeding implantation, must be operative.(30)
Trussell (2003) has noted that: "...our results suggest that inhibiting implantation of a fertilized egg is not the sole or primary mechanism of action ... we cannot exclude the possibility, however, that effects on the endometrium play a secondary role in the mechanism of action." (31)
Irrespective of how the Yuzpe method works at a molecular level, there is little debate that it greatly reduces the number of expected pregnancies. Ipso facto, this drug regimen cannot be classified as a contraceptive. It is a pre-implantation/emergency abortifacient.
(1) D'Hauterive P, Charlet-Renard C, Dubois M et al. What's new at the maternal-foetal interface: role of the hCG/LH-hCG receptor couple during embryo implantation. Rev Med Liege. 2006;61(10):705-12 (in French). The concept that human reproduction is a dual paradox is contained within the first sentence of the abstract (in English) from PubMed.
(2) Piccinni M-P. Role of T-cell cytokines in decidua and in cumulus oophorus during pregnancy. Gynecol Obstet Invest 2007;64:144-148
(3) Tissues transplanted from one person to another are called allografts. (http://www.mondofacto.com/facts/dictionary?allograft+rejection) Viewed February 23, 2010
(4) Piccinni, 2007, op.cit., p.147
(5) Piccinni, 2007, op.cit., p.146
(6) In the space of 12 hours, The Yuzpe method requires a woman to take 0.2mg of ethinyl estradiol (the synthetic estrogen) and 1 mg of levonorgestrel (the progestin). By comparison, Microgynon 30 contains 0.03mg of ethinyl estradiol and 0.15mg of levonorgestrel. This latter dose is ingested once every 24 hours.
(7) Simon C, Mercader A., et al., Hormonal Regulation of Serum and Endometrial IL-1α, IL-1β and IL-Ira: IL-1 Endometrial Micro environment of the Human Embryo at the Apposition Phase Under Physiological and Supraphysiological Steroid Level Conditions. J Reprod Immun 1996; 31: 165-84.
(8) Simon C, Velasco J, et al. Increasing uterine receptivity by decreasing estradiol levels during the preimplantation period in high responders with the use of follicle-stimulating step-down regimen. Fert Steril 1998; 70(2): 234-239
(9) Huang HY, Krussel JS, et al. Use of reverse transcription-polymerase chain reaction to detect embryonic interleuken-1 system messenger RNA in individual preimplantation mouse embryos co-cultured with Veto cells. Human Reprod 1997; (12): 7: 1537-1544
(10) Simon C, Gimeno MJ, et al. Embryonic regulation of integrins beta 3, alpha 4, and alpha 1 in human endometrial epithelial cells in vitro. J Clin Endocrinol Metab 1997;(82) 8:2607-2616
(11) Piccinni M.-P., Maggi E, Romagnani S. Role of hormone-controlled T-cell cytokines in the maintenance of pregnancy. Biochemical Society Transactions. 2000; 28:212-215
(12) Norwitz ER, Schust DJ, Fisher SJ. Implantation and the survival of early pregnancy. NEJM 2001;345:1440-1408
(13) Simon C, Velasco JJ et al. Increasing uterine receptivity by decreasing estradiol levels during the preimplantation period in high responders with the use of a follicle-stimulating hormone step-down regimen. Fert Steril 1998; 70 (2): 234-239
(14) Castelbaum AJ, Ying L, Somkuti S et al. Characterization of integrin expression in a well differentiated endometrial adenocarcinoma cell line (Ishikawa). J Clin Endocrinol Metab 1997; 82: 136-142
(15) Somkuti SC, Fritz MA et al. The effects of oral contraceptive pills on markers of endometrial receptivity. Fert Steril 1996; 65(3): 484-488
(16) Giudice L. Potential biochemical markers of uterine receptivity. Human Reproduction 1999; 14 (Suppl 2): 3-16
(17) Benton-Ley U, Sjogren A, Nilsson L. Presence of uterine pinopodes at the embryo-endometrial interface during human implantation in vitro. Human Reproduction 1999; 14 (2): 515-520
(18) Acosta AA, Elberger L, Borghi M, et al. Endometrial dating and determination of the window of implantation in healthy fertile women. Fert Steril 2000; 73(4): 788-798
(19) Duc-Goiran P, Mignot TM, Bourgeois C et al. Embryo-maternal interactions at the implantation site: a delicate equilibrium. Europ J Obstet Gynecol Reprod Biol. 1999;83:85-100
(20) Hambartsoumian E. Leukemia inhibitory factor (LIF) production by human deciduas and its relationship with pregnancy hormones. Gybecol Endocrinol 1998; 12(1): 17-22
(21) Ibid, p.20
(22) Giudice LC, Mark SP, Irwin JC. Paracrine actions of insulin-like growth factors and IGF binding protein-I in non-pregnant human endometrium and at the decidual-trophoblast interface. J Reprod Immun 1998; 38:133-148
(23) Han VK. The ontogeny of growth hormone, insulin-like growth factors and sex steroids: molecular aspects. Horm Res 1996; 45:1-2,61-66
(24) Giudice, op.cit., p.135
(25) Westwood M, Gibson JM, William JC, Clayton PE, et al. Hormonal regulation of circulating insulin-like growth factor-binding protein-I phosphorylation status. J Clin Endocrinol Metab 1995; 80(12): 3520-3527
(26) Suikkari AM, Tiitinen A, Stenman UH, Sepp M et al. Oral contraceptives increase insulin-like growth factor binding protein concentration in women with polycystic ovarian disease. Fertil Steril 1991;55(5):895-899
(27) Westwood M, Gibson JM, Pennells LA, White A. Modification of plasma insulin-like growth factors and binding proteins during oral contraceptive use and the normal menstrual cycle. Am J Obstet Gynecol 1999; 180:560-536
(28) Giudice, Human Reprod, p.11
(29) Swahn ML, Westlund P, Johannisson E, Bygdeman M. Effect of post-coital contraceptive methods on the endometrium and the menstrual cycle. Acta Obstet Gynecol Scand 1996; 75:738-744
(30) Mikolajczyk R, Spinnato II JA, Stanford JN. Uncertainty in estimating the day of ovulation causes overestimation of the role of ovulation disturbances on the effectiveness of the Yuzpe method of emergency contraception. Contraception 2003;68:69-71 (letter)
(31) Trussell J, Ellertson C, Dorflinger L. Effectiveness of the Yuzpe regimen of emergency contraception by cycle day of intercourse: implications for mechanism of action. Contraception. 2003;67:167-171
